Poster Presentation 5th Asia-Pacific NMR Symposium 2013
Brain viscoelasticity is associated with cranial venous drainage paths (#44)
Negative and low-pressure hydrocephalus are conditions characterised by the enlargement of the cerebral ventricles and, as the name suggests, negative or low intracranial pressure1. Insight into the condition has been aided by the advancement of phase-contrast cine magnetic resonance imaging (PC-MRI) but despite that, treatment remains difficult. Ventricular shunts are not always effective, even when programmed to operate at subatmospheric pressures. However, usage of a ‘neck wrap’ – an elastic bandage worn around the neck to compress the internal jugular veins – has been shown to reverse ventriculomegaly and restore neurological function through a postulated ‘stiffening’ of the brain tissue2,3,4,5. MR elastography (MRE) is an emerging non-invasive MR imaging technique that allows this property to be determined in-vivo. We aim to understand how jugular venous compression may affect the flow of ventricular cerebrospinal fluid (CSF), and how this in turn may affect the viscoelastic properties of the brain.
The effect of jugular compression on brain shear elasticity (G’) and viscosity (G’’) was assessed in nine healthy volunteers (3 female; 32.6 ± 10.9 years) using MRE. PC-MRI was used to assess cerebrospinal fluid (CSF) flow profiles in the cerebral aqueduct and blood flow in the neck.
Brain tissue elasticity and viscosity were linearly associated with the percentage of cerebral blood draining through the internal jugular veins (R2=0.475, P=0.040; and R2=0.449, P=0.048 respectively). The maximal caudal CSF velocity in the aqueduct increased significantly with jugular compression (t=-5.26, P<0.001). Jugular venous flow parameters were significantly reduced with compression while cranial arterial flow parameters were unaffected.
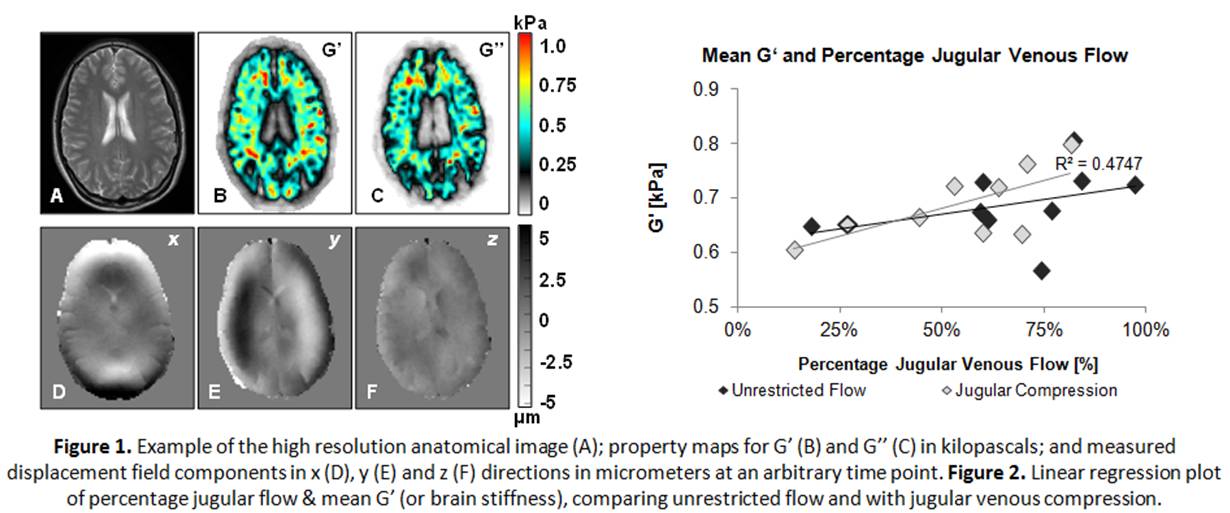
It is known that cervical compression creates increased resistance to cranial venous outflow and a subsequent increase in intracranial pressure6. This study is the first to show that cranial venous drainage paths following jugular venous compression correlate with the in-vivo viscoelastic properties of the brain.
- Pang, D. & Altschuler, E. Neurosurgery 35, 643–55; discussion 655–6 (1994)
- Rekate, H. Semin Pediatr Neurol 4, 167–78 (1997)
- Rekate, H., Nadkarni, T. & Wallace, D. J Neuros Pediatr 2, 1–11 (2008)
- Filippidis, A., Kalani, M., Nakaji, P. & Rekate, H. J Neurosurg 115, 1031–7 (2011)
- Wait, S., Ponce, F., Killory, B., Wallace, D. & Rekate, H. Clinical article. J Neuros-Pediatr 4, 217–21 (2009)
- Ho, A. M.-H., Fung, K., Joynt, G., Karmakar, M. & Peng, Z. J Traum 53, 1185–8 (2002)